- 1. Introduction to Neuroethics
- 2. Introduction to Neurotechnology
- 3. Neurotechnology and clinical research
- 4. Social Consequences of Neurotechnology
- 5. Future Directions
- 6. Neurotechnology in popular culture and popular imagination
- 7. Case Study
- 8. Conclusion
- 9. References
2. Introduction to Neurotechnology
Broadly, neurotechnology refers to technological innovations that alter brain function. The broad and diverse domain includes mechanical and surgical interventions such as implanted brain stimulators (as contrasted with medical or pharmaceutical interventions), medical treatment or neuroscience research methods of external brain stimulation with electricity or magnetism, and increasingly, includes brain-computer interfaces, implants that substitute for damaged sensory organs, and robotic devices. Frequently, the goal of neurotechnology is to bridge the gaps between the individual and his or her environment, and to ease communication and interaction between the two.
In this module, we briefly describe different types of advancing neurotechnologies, and their relevant ethical, legal, and social implications.
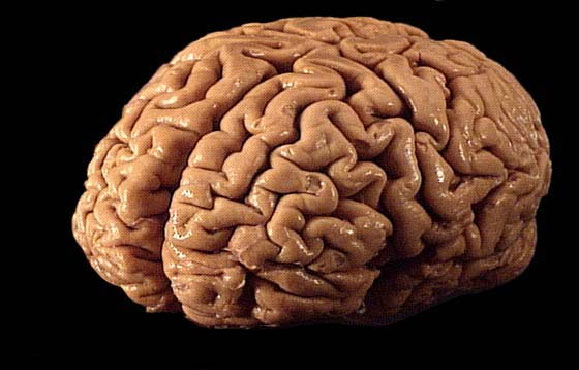
2.1. Augmenting signals coming into the brain

Source: Wikipedia
Much of the progress and success to date of neurotechnology centers around augmenting signals coming into the brain, enabling greater communication between individuals and the world around them. Devices that augment hearing are referred to as neural prostheses. The cochlear implant, as one example, allows hearing in people who are deaf by converting sound to something the brain can interpret, circumventing the sensory hearing mechanisms that are compromised. The implant includes a microphone and a speech processor that "transduces sounds to electrical signals that are applied directly to the cochlea via electrodes."2 Also under study is a similarly functional visual device that allows some vision for those who are blind. Also called an artificial retina,3 the device converts light into electrical signals to stimulate the retina. While the hearing device is functional and successful in enabling those who are deaf to hear, follow, and participate in conversations, the visual device is still in its early stages, although in early tests, people who are blind reported they were able to discern light spots that they could not without the device.
2.2. Decoding signals coming from the brain
Source: Mike Scioscia's Tragic Illness blog
Some neurotechnologies work to bring the outside world to an individual otherwise shut out because of dysfunctions with the sensory apparatus. Others look to bring the shut-in person back into communication with his or her environment. These devices can carry, decode, interpret, and act upon thoughts and brain waves that the person is not able to execute. This type of interface is used for people with paralysis due either to illness or injury. By thinking about the desired movement, interfaces allow individuals to control mechanical objects with their minds. These neuromotor prostheses circumvent the nervous system where the damage is located by picking up brain signals detected by electrodes placed on the cerebral cortex.4 Emerging through the skin, the electrodes connect to a series of computers. Successful experiments have enabled people to control their television sets, send and receive e-mail messages, move wheelchairs, and operate robotic arms -- all through brain-computer interfaces.

Source: HowStuffWorks.com
Robotic limbs are becoming increasingly complex and advanced. Touch Bionics, an upper-limb prosthetic company based in Scotland, was featured in the Washington Post in July 2007 for their i-Limb Hand. This device is the first marketed prosthetic to have individual motors at each finger joint. It allows for a previously unheard of range of motion, allowing users to accomplish tasks like turning a key or picking up delicate objects. The i-Limb Hand is controlled by nerve impulse signals delivered to the device through muscles in the arm.5
2.3. Brain stimulation
Source: Answers.com
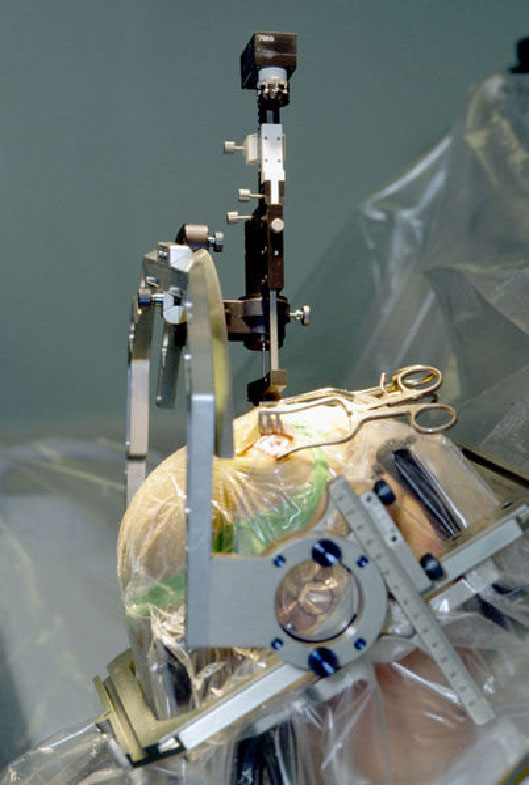
2.3.1. Deep Brain Stimulation
Persons with Parkinson's disease, or with disorders such as epilepsy, suffer from aberrant and uncontrolled movements, sensations, and behaviors due to disturbances in electrical brain functioning. Unlike past procedures where particular areas of brain tissue were ablated, Deep Brain Stimulation (DBS) aims to control involuntary movements using a thin electrode inserted deep into the brain to deliver a more regularly pulsed electric current, superseding the erratic pulses caused by the illness. This treatment has proven successful in many patients with movement disorders.
The electrodes for DBS reside deep in the brain. The electrical pulses -- the functional aspects of the device -- are regulated by a device similar to a pacemaker, inserted under the skin of the intraclavicular region. Like a pacemaker, its stimulation parameters are easily adjusted during a routine office visit. Such devices have been shown to greatly improve functioning in many of those who have been incapacitated by a movement disorder.
Under investigation is a newer prototype that, rather than emitting a constant and regular pulse, would detect an oncoming seizure through abnormal or arrhythmic brain waves. The device could then send out a regulating signal or pulse only when a seizure is imminent, making it both more efficient and more effective.
In addition to movement disorders, deep brain stimulation is being tested to treat depression and other psychiatric disorders including obsessive-compulsive disorder, anxiety, addiction, and eating disorders.6 In this use of DBS as a mode of neuromodulation, electrodes are inserted deep into the brain in order to "interrupt specific pathways between the frontal lobes and the deeper emotional parts of the brain, essentially 'rewiring' the brain."7
Because the electrodes are surgically placed while the patient is conscious, the effect can be noted immediately. Neurosurgeons can be certain of the correct placement by observing and monitoring the patient's physical reactions and changes in mood as the electrodes' positions change.
2.3.1.1. The Ethics of Deep Brain Stimulation (DBS)
Source: Neurosurgical Medical Clinic
As with most types of brain devices and manipulation, there is always the danger of adverse and unintended consequences. In the case of deep brain stimulation, the surgery itself carries a risk of damage to other parts of the brain. In using DBS for unremitting depression, we do not know for sure whether electrically modulating a "depression center" may hinder a person's social functioning or completely change the person's personality.
There is also the potential for misuse of the technique. Users may want the voltage on the device turned up to a level that might make the person proactively happy, rather than simply eliminating the depression. In cases such as this, users might want to adopt the procedure as a method of personal or performance enhancement. The risk of inappropriate expectations -- that patients who begin to respond may expect or wish the device to engender more wide-reaching positive changes in their psychological and social existence -- might drive such potential misuses or inappropriate desires. It is therefore very necessary, as in all such situations, to prepare patients to have realistic, scientifically guided expectations.
Finally, there exists the possibility that perhaps the state, in a dystopian futuristic scenario, could mandate that DBS or another implanted device forcibly be used to inhibit violent or criminal activity. Prohibitive cost, healthy medical ethics, public oversight, access to more conventional methods to try to shape behavior (including prison), and the inability of even sophisticated devices to tailor behavior to a specific pattern with certainty, make such scenarios unlikely. Nonetheless, it is important to be aware of the potential for such abuses, and to develop ethical guidelines that would make them very difficult to contemplate, let alone enact.
For some, the idea of brain surgery to implant a DBS stimulator brings up negative memories of the lobotomies that were very invasive, yet in their day, had been hailed as a miracle cure for the psychiatric patient. However, this would be an inaccurate comparison of two very different types of procedures. A form of psychosurgery, also known as a leukotomy (from Greek leukos meaning clear or white, and tomos meaning "cut/slice"), the lobotomy procedure involves cutting the connections to and from, or simply destroying, the prefrontal cortex. By severing neural connections in order to modulate behavior, lobotomies were used as salvage therapy for deeply disturbed individuals or to control unruly or socially unacceptable behavior. In many cases the lobotomized very-subdued, diminished patient also lost much sense of personal identity, the drive to achieve things in the future, and other aspects of basic human psychological status. Lobotomy surgeries were unregulated for decades. Only after forty years and tens of thousands of surgeries was the use of the lobotomy curtailed.
While some compare the action of DBS to the old-school lobotomies, there are many differences: the surgery to implant the DBS device is elective, although it may be prescribed inappropriately for some patients in the future. While it may sometimes have adverse surgical consequences such as unintended destruction of tissue, DBS surgery is not intended as a psychiatrically-controlling tissue-destroying procedure. Rather, it is a means to implant a very thin wire into a very specific brain area in order to stimulate and restore more normal affective functioning. The target brain area, for example in DBS for depression, has been identified based on extensive neurological and neuropsychiatric knowledge as the one most likely to have a pivotal effect on a complex brain network. Also, the effect of the DBS device on the brain can be reversed simply by turning it off. While in the future we may come to think of this intervention differently, and again, any potential for abuse is to be guarded against, the public would be mistaken to consider DBS surgery and lobotomy as directly comparable.
Nonetheless, it is important to consider both the history of psychiatric neurosurgery and the implications of the present and future effects of the current methods. Some fear that the rush toward DBS to treat myriad conditions, not all of them medical, may result in more heartaches and headaches than DBS can cure. Additionally, neurosurgeries ignore underlying psychological issues, treating the symptoms rather than the causes of depression, obsessive behavior, or other maladies. We must acknowledge that to date, like electroconvulsive therapy (ECT), the exact mechanism of action of DBS remains elusive. There may be solutions to psychiatric disorders that are less drastic than brain surgery and the permanent implantation of an electrical regulating device. While DBS may be a perfect fit for particular problems in carefully selected individuals, DBS is not a perfect fit for all psychiatric and neurological problems, and caution is advised before racing to use the most advanced technology in all cases.
2.3.2. Transcranial Magnetic Stimulation (TMS)
Transcranial Magnetic Stimulation (TMS) is another method of brain stimulation. Rather than implanting electrodes directly into the brain, TMS works by delivering very brief single pulses, or brief rapid trains of pulses of a strong magnetic field created by electrical wires contained in a housing device. The device is held in place by a human operator, or in a mechanically fixed position, at the surface of the skull. The magnetic field induces an electrical charge and a current in the local neural areas in the brain directly under where the device is positioned, although the neural activation then can spread somewhat to other regions of the brain. Target sites for stimulation are chosen according to theory and evidence about brain functional networks. Placement is guided by fMRI images of the brain and frameless stereotaxic software that maps from the brain image to the individual's head. Depending both on stimulation sites and frequencies of stimulation delivered (typically from 1 to 30 Hz, but sometimes higher), the TMS device can either stimulate (excite) or reduce (inhibit) local areas of neural activation.

Source: Science Museum
The ability of TMS to neuromodulate flexibly means that it is a possible therapy for a range of neuropsychiatric conditions (e.g., depression, schizophrenia, obsessive compulsive disorder, autism), and also is a valuable tool in neuroscience research, where it can be used to explore many aspects of interconnectedness and function within the brain. TMS also is useful in studying the motor fibers that connect the brain with the spinal cord. Clinically, it also provides diagnostic and prognostic insights for those with motor neuron disease such as amyotrophic lateral sclerosis (ALS or Lou Gehrig's disease), multiple sclerosis, stroke, and spinal cord lesions.8
In the future, TMS technology may offer insights into the pathophysiology and pharmacology of Parkinson's disease, or provide pre-surgical evaluation through non-invasive cortical mapping. TMS could be used as a rehabilitation method for motor neglect problems, stroke, or aphasia.9 While human and animal studies indicate TMS is less effective for major depression than electroconvulsive therapy (ECT), TMS may provide an alternative to treating less severe depression, one that is less invasive than ECT and does not cause the kinds of memory problems frequently seen after ECT. Unlike ECT, TMS is not intended to cause a seizure in patients (the seizure process during ECT is therapeutic for the depressed individual). Still an experimental therapy, when TMS is used in clinical or neuroscience research studies, persons who may be at risk for seizures are excluded. Safety guidelines for the stimulation parameters of TMS also mean that unwanted seizures and other undesired side effects are very infrequent.
Another, newer experimental therapy is Magnetic Seizure Therapy (MST), in which the magnetic stimulation is delivered transcranially but at stronger doses than in TMS. In MST, as in ECT, a seizure should be created for therapeutic action in severe depression. Thus far, animal studies and very limited human data suggest that MST may be an alternative to ECT for severe depression, but much more research is needed to establish the safety and possible efficacy of MST.
In addition to the therapeutic uses listed above, TMS experiments have shown the potential for neural enhancement. After receiving TMS as participants in experimental studies, individuals free from neural disease or defect have experienced increased finger-reaction time, as well as positive changes in memory, abstract thinking, color perception, motor learning, perceptual learning, and increased abilities in drawing and language.10 TMS is being studied for its possible benefits in reducing the impact of sleep deprivation. On the other hand, many cognitive or other responses of study participants in types of TMS protocols involve temporarily interrupted or diminished capacities. The impact of TMS on behaviors is very dependent on the brain site of stimulation, the duration and intensity of stimulation, and when the stimulation is delivered relative to a task the study participant is performing. Currently, both the positive and negative impacts of a TMS session are observed to be very short-lived: it may be gone immediately after stimulation ceases, or within a few hours. Nonetheless, especially as this technology and knowledge of how to use it advances, the possibility exists that it could be used for types of neural or performance enhancement for which it was not intended.
2.3.2.1. The ethics of Transcranial Magnetic Stimulation (TMS)
Although the literature is replete with discussions of experimentation and efficacy regarding internal and external brain stimulation, as this field is relatively new, to date few controlled studies have been published. Because of the complexity of the brain and our still meager understanding of its mechanisms and operations, current understanding of how one might achieve optimal stimulation is still very limited. Continued development of the above brain stimulation technologies, and others including low-frequency ones such as tDCS (transcranial Direct Current Stimulation) and CES (Cranial Electrotherapy Stimulation), will guide both relevant clinical and research applications, and ongoing discussion of the ethical issues involved in their use.
2.4. Intra vs. extra cranial devices
Intra-cranial devices, compared to extra-cranial devices, offer the benefit of a more permanent, and perhaps more exact solution to neurological disorders, yet there are many concerns with their use. First, intra-cranial devices carry more risk because brain surgery is needed to insert them. Additionally, the reversibility of an implant is complex as it requires additional surgery and the risk of unforeseen complications that result from removal of a device that has become a part of the person's brain. Of great concern is that there are no long-term follow-up data on the effects of having a device permanently implanted in the brain.
3. Neurotechnology and clinical research
Research and development of any new devices is both an opportunity for brain science and clinical care to advance, and a serious challenge for the medical and wider communities to address any dangers and complications, ethical and moral quandaries, and issues of healthcare economics and distributive justice. In the case of neurotechnologies, these potential pitfalls are considerable, as intervening in the brain is always fraught with potential for serious consequences. Despite these concerns, only with carefully conducted clinical and experimental studies can we push the envelope to advance care for people with brain, emotional/psychological, or neuropsychiatric disorders.
3.1. Study populations and issues of informed consent
Finding subjects/participants willing to participate in a research study given the potential risks and benefits of the intervention under investigation can be challenging. In recruiting patient volunteers for neurotechnology protocols, it must remain clear that many of these interventions are salvage therapies, used only with patients for whom neither traditional nor more aggressive treatments have been effective in mitigating their disease or symptoms. These people are likely to be desperate, willing to try any novel device that offers the possibility of a cure, or even relief from suffering. Neurology patients whose disorders are refractory to conventional treatment may also have cognitive deficits and so be unable to give fully informed consent if they cannot adequately process the risk information and consequences of the novel procedure. People on the edge of capacity may know that they want to get better, but may not understand the risks of getting there.11

Source: HSE UK
Researchers must recruit healthy volunteers to better understand how the healthy brain looks and functions. Still, risks to healthy volunteers undergoing neurological intervention investigations are uncertain, while the potential for benefit as a result of the intervention in these cases is negligible. Using TMS, for example, researchers can create in a healthy volunteer a short-lived "virtual lesion" to study the function of the brain without relying only on the effects of disease and disaster to yield these kinds of insights. What should trouble researchers are the limitations to our knowledge of neural plasticity. We know little about how long any changes induced by TMS may endure, or what the long-term consequences might be.
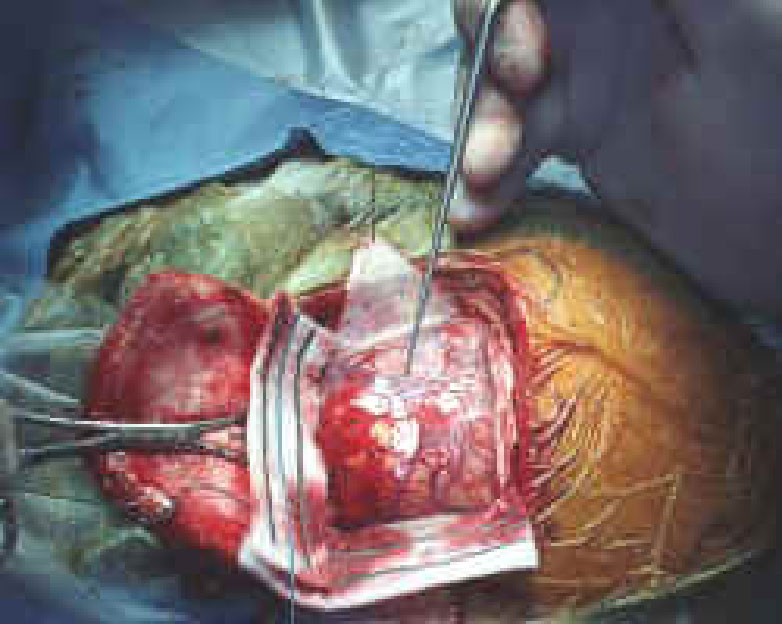
Diverse neuroscience and clinical investigations of the brain via a range of devices and methods continue to evolve. Future generations of brain imaging and brain stimulation devices will undoubtedly offer us much more precision with fewer (we hope) risks and problematic elements. Given the state of current technology, many brain surgeries are performed on conscious patients who can respond in real time and alert surgeons to intended as well as unintended and unanticipated casualties of the brain manipulations. Again, people who are sick and desperate for relief may be willing to take these risks, but ethically, should we allow them to? Similarly, can we allow otherwise healthy people to participate in trials and put themselves at risk?
Studies conducted at scientifically appropriate sites have in place extensive means to minimize risk to participants, via extensive review of research protocols by Institutional Review Boards (IRBs), by employing extensive inclusion and exclusion criteria for participation that screen out those most at risk for a complication of participating, as well as other safeguards. Nonetheless, problems and unintended consequences may arise. Yet to prevent brain stimulation studies from going forward essentially will restrict the advancement of critical knowledge. Comprehensive safeguards and constant vigilance are always needed if studies are to proceed that place research volunteers or patients at risk.
3.2. Placebo-controlled (sham) surgeries
The double-blind, randomized (placebo) controlled trial (RCT) has been upheld as the gold standard for medical research. Although the research ideal, it can be clinically problematic and perhaps unethical to withhold necessary and proven, or even promising experimental treatment, from a patient in need who has volunteered to participate in a research study and ends up in the placebo-controlled arm.
There have been published reports of placebo controlled surgeries (also known as "sham surgeries"), whereby surgeons make burr holes into the skull as if they were implanting an electrode, fetal tissues, or other intervention, yet do not follow through with the final stage of the surgery.12 Some suggest that if one needs a placebo surgery to satisfy the investigational research design, a device can be implanted and left off, to be turned on at a later date, after review of positive efficacy data. This does not anticipate, however, the RCT where, after analyzing study data, we learn that the device or implant itself is detrimental to health or quality of life. Needless to say, we do not want to have inserted dummy devices into the brains of individuals who not only have no chance of benefit, but also now have a greater chance of harm from its placement. Additional risks are incurred in this instance when the study participant must undergo additional brain surgery to remove the dummy device.
Another potential quandary of placebo surgeries may arise if a neurosurgeon performs a procedure in an attempt to appease a desperate or irrational patient.13 Because of increased numbers of patients educating themselves and feeling a greater sense of empowerment, more patients are likely to demand specific treatment from their doctors such as tests, prescription medications, or even surgeries. This is an opportunity for reasoned discourse and explanation to the patient of the harms and benefits of any intervention, and how these forces balance in the particular case of this patient.
3.3. Safety
A critical ethical consideration in brain-computer interfaces is the lack of clinical oversight and systematic review of successful data (e.g., a Cochrane or Agency for Healthcare Research and Quality (AHRQ) review). There is a plethora of anecdotal evidence noting the success of brain devices, but scant published data from randomized controlled clinical trials and almost nothing (as usual) detailing unsuccessful trials. This is due in part to the complexity of both the brain and the mind. There are no accurate mapping programs to follow to confirm that two patients have received identical procedures. Even if they received identical procedures, the myriad connections and pathways in the brain are likely to yield different results from the ostensibly same intervention.
4. Social Consequences of neurotechnology
4.1. Therapy vs. enhancement

Source: European Commission - IST Event 2004
Neurotechnological interventions aim to restore or repair deficient or dysfunctional capabilities. Brain science has been able to provide artificial hearing for those who are deaf, some vision for those who are blind, improved emotional status and better mental focus and functioning for those with emotional and personality disorders, and more controlled motor skills for patients with Parkinson's disease and other movement disorders.
There is considerable debate, however, concerning treating normal variations in the population as opposed to treating bone fide diseases. Many in the deaf community, for example, argue that deafness is not a disease, that deafness is a human variation like many others, and that the deaf are healthy people who simply do not hear well. With the advent and popular use of cochlear implants, the deaf community sometimes has objected to the use of implants to improve hearing, as though deafness were a deficiency or disease to be corrected or healed. They maintain that theirs is a distinct culture with its own language and customs, and that cochlear implants negate who they are and decimate their community, via this medical attempt to make them more like normally-hearing persons.
While their perspective may be valid, it is likely that some spokespersons against cochlear implants do not represent the views and opinions of the total deaf community. While a deaf couple may be proud of who they are and decide against the implant for their hearing-impaired child in the name of heritage and community, their child may grow up to disagree with that belief and resent their parents for making that decision. Many individuals who are deaf simply want to optimize their or their family members' possibilities for communication and learning, both within and without the deaf community.
People draw a distinction among the different degrees of intervention to alter one's vision or hearing. Few argue against people wearing glasses or hearing aids, or having an artificial joint, if medically warranted. The conflict seems to arise only in the case of brain manipulation, as the fear is that placing a device or implant into the brain changes who we are as individuals and exerts a fundamental and irrevocable influence on our personhood.
The fear of being altered via outside agency by devices or even drugs is very deep-seated within us. Many people with types of mental illness, for example, have delusions that there are implants in their brains or bodies that are communicating with or controlling them, almost always in a negative way. However, as human beings continue to evolve in an increasingly sophisticated technological world, even these very fundamental human perspectives gradually may change.
4.2. Fair distribution of resources
As the technology advances, if we allow or encourage brain-computer interfaces, for example, for those with sub-standard performance in a given domain, where do we draw the line that defines what is "standard?" For the person who is "average," or just barely above the cutoff for an intervention, should an enhancement be offered to provide a compensatory boost or competitive edge? Another consideration for enhancement is the concern that an increase in efficiency or ability in one attribute may cause a decline in another. One can not predict how changing one's natural skill set via artificial means will affect the person as a whole.14

Source: BBC Online
People who compete at a higher level, where any advantage offers an edge, may be willing to pay dearly for enhancement. The controversy over the use of steroids and other drugs and boosting techniques in sports is a prime illustration, if mostly in the non-neural realm, to date. Athletes both elite and ordinary will risk their health, and sometimes sanity, achievements, and reputations, in the quest for ever more perfection or competitive advantages. In such contexts, is even medically supervised brain modulation or enhancement ethical?
Many other problems will arise. If some of these brain-enhancing procedures and implants ever become available for purchase, some who have a disability may seek to be able to elevate their performance to that of the average person. Very likely, however, they would still remain far below the new "average" or standard for enhanced states. This could lead to, among other things, a diminished sense of personal reward, after sacrifice or transformation, with little gain of happiness or betterment.
Consider if, in the future, athletes, chess players, Wall Street titans, and other high level competitors try to gain unfair advantage through brain enhancement. If they were to succeed, how would society understand or "regulate" their successes and manage the probable desire of many others to follow suit? What are the implications of joining one's body to brain devices via means and for ends that today we regard as suspect, or even dangerous, and against our Western ethical and religious traditions? In the future, we may come to feel differently. If fairness ultimately may demand equal access to enhancing techniques, then our society may evolve to the point where many types of enhancement are approved of and made more universally available. From the perspective of today, this is an unsettling vision.
Those who support increased access to and acceptability of enhancement therapies argue that we already work hard to enhance our bodies and our minds. We go to school and take master classes. We exercise and practice difficult skills until they become easy.
Source: Answers.com
"Neuroplasticity" is the term used to describe the ways in which the brain is changeable and teachable, through practice- and mastery-based behavioral means as well as through mechanical or psychiatric means.15 Given this reality, then using more external and artificial means of brain transformation is simply a different path to the same desired and enhanced outcome. Using a multidisciplinary approach, we will need to develop guidelines that determine an "acceptable standard" for improvements, enhancements, or interventions in the brain.
Newer neurological devices are more accurate and serve patients better, but are more expensive and require greater skill and care to implant. The poor and disenfranchised are less likely to have access to these devices, yet may have a greater need for them as a consequence of their disproportionate share of illness. If the upper levels of society have access to improved devices and treatments, then the poor will be at an even further disadvantage if they receive fewer or less sophisticated interventions. As an example, in the case of deep brain stimulation for depression, the poor are more likely to be depressed, but less likely to be able to access this kind of treatment.16
5. Future Directions
We anticipate very positive outcomes will evolve from neuron-stimulating devices and brain-computer technology and research. While deep brain stimulation technology currently provides only a steady pulse of electricity, regardless of how much the person needs, a future improvement will allow for detection of need and then pulse only when necessary, reducing the burden of the device on the individual. This type of interactive and responsive programmability is already here for an experimental device to control epilepsy. Similarly, a future device could detect levels of medications and other substances in the blood, triggering needed time-released medicines. Advances in brain devices may also provide feedback mechanisms so the brain can change and adapt to meet the needs of robotics or other therapeutic devices.
Since the earliest computer incarnations, people have feared a coming revolution, when computers and robots might replace, or rule, human thought, action, and even feeling. Each new neurotechnological innovation has the potential to advance us toward a state of technophobia, a fear of unforeseen problems, as well as a state of overconfidence in the promises of the innovations. We need to remember that technology is a tool that we as individuals decide how and when to use and incorporate into our lives. It is our obligation, as human beings, as scientists, and as bioethicists, to remain focused on the positive and minimize the fear of the negative. We must also develop deeper knowledge and understanding and elaborate guidelines and standards that reflect desired constraints. Only then can we achieve the desired many-faceted goals for our highest aspirations with regard to the use and development of brain-modulating and other technologies.
6. Neurotechnology in popular culture and popular imagination
Popular fiction jumps often to the wildest extremes when contemplating emerging neurotechnologies. Some examples from "pop culture" are truly figments of fertile imaginations. Yet, what writers and directors dream up that is virtual today may well become reality in the future.
6.1. Eternal Sunshine of the Spotless Mind
In the 2004 movie, Eternal Sunshine of the Spotless Mind, the main characters undergo advanced technological procedures to erase both their painful and pleasant memories of each other after their relationship sours. The truth they find is that only through experience, and our memories of these experiences, do we become who we are. While the movie shows selective memory elimination, current memory-erasing technology does not exist, except in fiction, and of course in the real world as a consequence of serious illness (e.g., Alzheimer's disease) or trauma (e.g., traumatic brain injury; planned or accidental surgical ablation).
One cannot simply excise memories of a specific individual, or of specific experiences, from one's long-term memory. Some drugs, investigated only in controlled experimental settings, may be able to prevent the creation of memories tinged with unpleasantly strong feelings, but only if taken immediately before the traumatic or unpleasant exposure. These drugs work by blocking types of co-occurring neural signals that link a specific memory and the feeling present at the same time. Some behavioral or brain stimulation interventions may be capable of helping people to train their brain function so as to change some of the negative after-effects of traumatic experiences, to enable a person to experience things differently, and to recover and change. This is very far from being able to alter specific memories, although some will be changed in their emotional strength or other aspects of remembered detail. Currently, types of totally non-technical psychotherapy, or meditation, help people to change their inner experiences and hence also affect aspects of their memories.
While in the short term, we may want to permanently delete memories of our negative and painful experiences, in the long run, that might not be a benefit if these memories define and shape our personalities, beliefs, and values, and teach us valuable lessons.
Source: IMDB.com
6.2. Harrison Bergeron
In the short story by Kurt Vonnegut, Jr., Harrison Bergeron lives in a dystopic world that uses brain and body devices and implants in an attempt to make everyone equal. However, instead of raising everyone up to the highest standard, the government chooses instead to lower people to the lowest common denominators of human thought and action. People with beautiful faces wear hideous masks. People with above-average intelligence wear a "mental handicap radio" device that gives a soul-shattering piercing noise directly into the ear to destroy any train of thought. Larger and stronger people have bags of buckshot padlocked around their necks. The goal of the handicapping program is that people not feel badly about themselves if they see someone "better" than they are. At the climax of the story, an extraordinarily tall, strong, handsome, and smart boy breaks through all his handicaps and declares himself emperor. Not only is he naturally stronger and more capable than everyone else, but without his handicaps he is especially so. When the government destroys him soon after his uprising, no one, not even his parents, can remember who he was or what he did, because no one can think or reason better than the least naturally capable person.
Source: Rensselaer Polytechnic Institute
6.3. Flowers for Algernon
In Daniel Keys' 1953 short story "Flowers for Algernon," Charlie is a mentally retarded adult who undergoes brain surgery to make him smarter. His companion in the experiment is a small white mouse named Algernon who had the same surgery a few weeks before Charlie and acts as a bellwether, foretelling Charlie's fate and outcome. As Charlie becomes smarter, his personality changes dramatically. No longer is he an easy-going fellow who works as a janitor and has a friendly smile for all. Suddenly, he is suspicious, haughty, self-righteous, intolerant, and hostile to all his associates and former friends. All this serves to alienate him from everyone in his world. It is rather clear that his associates' discomfort is partly because Charlie has suddenly become so much smarter than they are, and partly because he rather abruptly stops being who he was. Changing his intelligence changed his personality so drastically that no one could adapt to him. After Algernon's death, following a rapid decline in his enhanced intelligence, an autopsy confirms that neural enhancement is only temporary, and its receding effects leave the subject not at his pre-surgery mental state but in a considerably worse situation than the one in which he started.
Please click here to go to the interesting cases and challenging questions.
1 Van Essen DC. Introduction. The Dana Alliance for Brain Initiatives. 2007 Progress
Report on Brain Research. New York: Dana Press; 2007.

2 Foster KR. Engineering the brain. Neuroethics: Defining the Issues in Theory, Practice,
and Policy (J Illes, ed.). New York: Oxford University Press; 2006.

3 Foster KR. Engineering the brain. Neuroethics: Defining the Issues in Theory, Practice,
and Policy (J Illes, ed.). New York: Oxford University Press; 2006.

4 Ackerman, SJ. Hard Science, Hard Choices: Facts, Ethics, and Policies Guiding Brain
Science Today. New York: Dana Press; 2006.

5 Hom K. With This Hand, Actions Speak as Loud as Words. Washington Post. 2007 July
31. Available from: http://www.washingtonpost.com/wp-
dyn/content/article/2007/07/27/AR2007072702111.html.

6 Egan D. The New Lobotomy? 'Deep brain stimulation' tested at UBC as depression
cure. The Tyee: A Feisty One Online. 2007 Oct 26. Available from:
http://thetyee.ca/News/2006/10/26/DBS/.

7 Egan D. The New Lobotomy? 'Deep brain stimulation' tested at UBC as depression
cure. The Tyee: A Feisty One Online. 2007 Oct 26. Available from:
http://thetyee.ca/News/2006/10/26/DBS/.

8 Steven MS, Pascual-Leone A. Transcranial magnetic stimulation and the human brain:
an ethical evaluation. Neuroethics: Defining the Issues in Theory, Practice, and Policy (J
Illes, ed.). New York: Oxford University Press; 2006.

9 Steven MS, Pascual-Leone A. Transcranial magnetic stimulation and the human brain:
an ethical evaluation. Neuroethics: Defining the Issues in Theory, Practice, and Policy (J
Illes, ed.). New York: Oxford University Press; 2006.

10 Steven MS, Pascual-Leone A. Transcranial magnetic stimulation and the human brain:
an ethical evaluation. Neuroethics: Defining the Issues in Theory, Practice, and Policy (J
Illes, ed.). New York: Oxford University Press; 2006.

11 Foster KR. Engineering the brain. Neuroethics: Defining the Issues in Theory, Practice,
and Policy (J Illes, ed.). New York: Oxford University Press; 2006.

12 Freed CR, Greene PE, Breeze RE, Tsai WY, DuMouchel W, Kao R, Dillon S, Winfield H,
Culver S, Trojanowski JQ, Eidelberg D, Fahn S. Transplantation of embryonic dopamine
neurons for severe Parkinson's disease. N Engl J Med. 2001 Mar 8; 344(10): 710-9.

13 Ford PJ, Henderson JM. Functional neurosurgical intervention: neuroethics in the
operating room. Neuroethics: Defining the Issues in Theory, Practice, and Policy (J Illes,
ed.). New York: Oxford University Press; 2006.

14 Ackerman, SJ. Hard Science, Hard Choices: Facts, Ethics, and Policies Guiding Brain
Science Today. New York: Dana Press; 2006.

15 Zuger A. The Brain: Malleable, Capable, Vulnerable. The New York Times. 2007 May 29.

16 Ackerman, SJ. Hard Science, Hard Choices: Facts, Ethics, and Policies Guiding Brain
Science Today. New York: Dana Press; 2006.

17 Appelbaum PS, Lidz CW. Re-evaluating the therapeutic misconception: response to
Miller and Joffe. Kennedy Inst Ethics J. 2006 Dec; 16(4):353-66.

References for Sidebars
S1 Sabbatini RME. The History of Lobotomy. Brain and Mind: Electronic Magazine on
Neuroscience. 1997 June; [cited July 2, 2007]. Available from:
http://www.cerebromente.org.br/n02/historia/lobotomy.htm.

S2 Weil M. Rosemary Kennedy, 86; President's Disabled Sister, Obituary. Washington Post.
January 8, 2005. B6. Available from: http://www.washingtonpost.com/wp-
dyn/articles/A58134-2005Jan8.html

S3 Dully H, Fleming C. My Lobotomy - A Memoir. New York: Crown Publishers; 2007.

S4 Blumenfeld H. Neuroanatomy through clinical cases: Neglect and constructions. [cited 2007
July 9]. Available from: http://www.neuroexam.com/content.php?p=10.


