
 |
Early Childhood Caries
Learning Objectives
- State the goal of early intervention and importance of the “dental home”
- Define dental caries (tooth decay)
- Differentiate early childhood caries from dental caries generally
- Explain the transmission and colonization of bacteria associated with early childhood caries
- Characterize the prevalence and consequence of early childhood caries
- Describe conventional treatment for early childhood caries (restorative dentistry)
- Describe emerging disease management for early childhood caries
In This Section
You meet Mrs. Perez' daughter, Maria and follow her oral health through her second year of life.
Table of Contents
The Child: Maria Perez - 12 Months
Why should Maria's physician refer her to a dentist?
The Child: Maria Perez - 33 Months
Failure of Early Intervention?
What is Dental Caries?
What is Early Childhood Caries?
Maria's Reality
The Child: Maria Perez - 12 Months
During Maria's 12-month well-baby exam at her primary care physician's office, Mrs. Perez reports that Maria's front teeth “didn't look right” when they first came in. The health history indicates that Maria was a pre-term infant (i.e.. < 37 weeks gestation) with a low birth weight (i.e.. < 2500gm). Her physician takes a brief look, reassures Mrs. Perez that the dental appearance may be a “developmental problem” and suggests that if she has further dental concerns, that she should consult a dentist. The primary care provider, unaware of the American Academy of Pediatric's Infant Oral Health Guidelines, does not provide oral health risk assessment or counseling and does not facilitate a formal referral as is typically done for other types of services.
As young as Maria is, both developmental and acquired disease are already evident on careful examination.
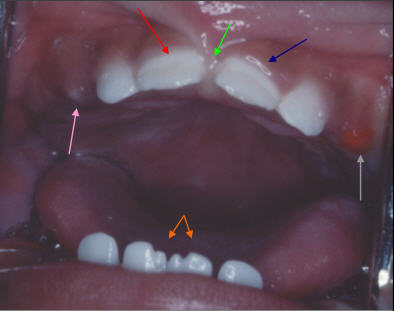
Active Disease:
- RED Arrow: thick plaque and decalcification (mineral loss) on primary teeth
- BLUE Arrow: shows the gingival tissue as shiny and full, indicating inflammation
Developmental Findings:
- ORANGE arrows: Notching of incisors
- GRAY arrow: eruption hematoma
- PINK arrow: atypical eruption sequence
- GREEN arrow: anatomical variant of the labial frenum

Place Mouse on Question to Reveal Answer
The primary components of dental plaque are bacteria, inter-bacterial matrix, and debris. Acid, produced by many bacterial species (especially the mutans Streptococci) concentrates in the plaque and destroys the tooth surface by “decalcifying” the enamel. Plaque may be especially concentrated in surface defects such as those associated with prematurity. Twenty percent of remature children like Maria have such enamel hypoplasia which is defined as a deficiency in enamel formation, that manifests clinically as grooves or pits, or a lack of surface enamel (29).
Why should Maria’s physician refer her to a dentist?
The goal of an early dental assessment is primary prevention. This may be accomplished with the timely delivery of oral health information, including the conditions that create caries & cavities; its natural progression; and its prevention (read more about "Anticipatory Guidance" later in this module), and the identification of populations at high risk for tooth decay. The traditional approach of treating the effects of tooth decay (i.e.. “drilling and filling”) can be replaced by disease prevention and disease management if children at high risk of developing cavities can be identified early and effectively.
Prevention focuses on the establishment and maintenance of good oral hygiene, optimizing systemic and topical fluoride exposure, and eliminating high frequency or prolonged exposure to simple sugars in the diet. Prevention is the foundation for the establishment of a “dental home” by 1 year of age. The concept of the "dental home" as advocated by the American Academy of Pediatric Dentistry is derived from the American Academy of Pediatrics concept of the "medical home." This concept states that “the primary health care of infants, children, and adolescents should be accessible, continuous, comprehensive, family centered, coordinated, compassionate, and culturally effective. It should be delivered or directed by well-trained child health specialists who provide primary care and help to manage and facilitate essentially all aspects of pediatric care” (25).
Every child should have an examination and oral health risk assessment by 12 months of age by a dentist or qualified pediatric health care professional. (26) The Caries Risk Assessment Tool (CAT), provided by the American Academy of Pediatric Dentistry (27), was designed to assist both dental and other health professionals in assessing the risk of tooth decay in infants, children and adolescents. Questions directed at dietary practices, fluoride exposure, oral hygiene, utilization of dental services, socioeconomic status and general level of health can help determine if a child is at low, moderate or high risk for dental disease.
Using the CAT, and Maria's history (low socioeconomic status and no usual source of dental care) and exam findings (thick plaque, areas of demineralization and gingivitis), Maria would be considered at high risk for dental disease.
It is too late for Maria to gain the advantage of primary prevention and some aspects of anticipatory guidance, as she already exhibits overt signs of dental disease. Maria, however, is not too late for disease suppression. With proper diet control and the application of topical fluoride, Maria may avoid surgical intervention if timely care is obtained. Unfortunately, without a timely dental referral to a dentist who will provide disease management services, disease progression is inevitable.
The referral was never made from Maria’s physician to a dentist and Mrs. Perez failed to negotiate the dental care system on her own.
The Child: Maria Perez - 33 Months
Maria is now 33 months old and has presented with her mother to the local health center dental clinic, because, according to Mrs. Perez, Maria has “been up all night, crying about her teeth”. (See image of Maria's teeth at left, click to enlarge)
Dental History - in the last 2 months, Maria has become increasingly irritable at mealtimes. It began as whining with cold or sweet foods, and has progressed to crying when biting with the front teeth. For the last 3 nights Maria has awoken from sleep and Mrs. Perez has been able to console her with her usual bottle of apple juice. Last night, she was inconsolable and required pain medicine (“baby Tylenol”) to help her sleep.
Mrs. Perez, aware of Maria's problem, had elected to “wait it out” in part because of her physician's statement that the poor appearance of the teeth represented a “developmental problem” and in part because she felt since these are “baby teeth”, that they will “just fall out sooner or later”.
Failure of Early Intervention?
Tooth decay in the primary teeth, has significant functional and disease progression consequences:
Disease: Since the mouth (rather than any single tooth or tooth surface) is the locus of disease and not all the primary teeth are replaced simultaneously, disease in the primary teeth will set the stage for decay in the incoming permanent teeth. Dental disease impacts all these new teeth as they become available, and because the exchange takes so long (until age 12-13 years), children that have untreated, active oral disease are at an increased risk for more generalized, ongoing and often severe tooth decay.
Child: As can be seen in Maria's case, early childhood tooth decay in the primary teeth, if not cared for, results in chronic pain, infection and sleeplessness. It may also lead to poor weight gain, the inability to eat (2) and may affect the overall quality of a child's daily life. (30)
Dentition: Loss of primary teeth impairs mastication, affects the development of the craniofacial system, and results in loss of arch space for the succeeding permanent teeth to “grow in” (erupt) into the proper position. This is the reason that failure to maintain the primary dentition intact leads directly to orthodontic problems as the permanent teeth replace them.
Maria is diagnosed with severe early childhood caries
(early childhood tooth decay).
What is Dental Caries?
Dental caries, better known as “tooth decay”, is the disease process that leads to the loss of tooth mineral and eventually to cavitation of the tooth surface (“cavity”). It is a dieto-bacterial, infectious, transmissible, oral disease. Three things are required for dental caries activity to become established and progress: one or more susceptible tooth surfaces, "cariogenic“ (decay causing) bacteria, and fermentable carbohydrates (particularly sucrose).
“Tooth Decay” refers to both the process and result of dental caries. |
|
What is Early Childhood Caries?
Early Childhood Caries (ECC) or early childhood tooth decay, previously termed “nursing caries” or “baby-bottle tooth decay”, is a particularly virulent form of tooth decay that affects the teeth of infants and preschool children. Its formal definition, as stated by the American Academy of Pediatric Dentistry (AAPD), is based on the age of the child when decalcifications or cavities are first noted. ECC is diagnosed when any child younger than “71 months” demonstrates any sign of tooth decay or prior treatment for tooth decay. Severe ECC is diagnosed when a young child has evidence of tooth decay on multiple teeth. Since AAPD's definition was adopted in 2003, greater attention has been placed on younger-and-younger children so that any child under age three with any sign of tooth decay should be considered to have the severe form of ECC.
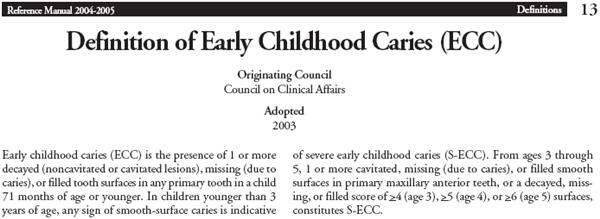
Source: http://www.aapd.org/media/Policies_Guidelines/D_ECC.pdf
ECC Etiology: The process of ECC is the same as the generic process of tooth decay: a combination of acidogenic bacteria that metablize simple carbohydrates into acid thereby producing an environment on the tooth surface that decalcifies tooth structures until they are so weakened that they collapse into a “cavity.” What distinguishes ECC and especially Severe-ECC (S-ECC) from ordinary tooth decay is its aggressiveness. This enhanced pathogenesis is primarily predicated on the contribution of specific “cariogenic” (decay causing) bacteria in the dental plaque. (Dental plaque is the sticky white or yellowish film of bacteria, bacterial products, and debris that forms on tooth surfaces, especially along the gum line where it is least disturbed by eating and brushing). In particular, the plaque that causes ECC and S-ECC is richer in bacteria of the mutans streptococci group as these bacteria are the most efficient and effective in initiating the caries process. Children with ECC have “mutans” levels in plaque that typically exceed 30% of the plaque's bacterial composition (31-33) while young children without ECC have plaque with mutans that compromises less than 1% of cultivable flora (34). Based on over 35 years of experimental and clinical studies, the mutans streptococci have been implicated as the primary infectious agent for caries initiation.
Transmission and Colonization: Infants' teeth are colonized with bacteria, including those that promote caries, shortly after the eruption of the first primary teeth at approximately 6 months of age. Colonization requires direct transmission of saliva from the primary caregiver, typically the mother, to the child. This transmission occurs whenever and however saliva is “shared,” for example by using the same spoon to taste and feed a baby, by maternal cleaning of a pacifier in her own mouth before passing it to the child, by using saliva to clean around a baby's mouth, or during play through which the baby picks up maternal saliva on its hand or face and transfers the saliva to its own mouth. As with other infectious conditions, the “success” of transmission depends on three factors:
- The Source, i.e. the titer of the inoculum: in this case the concentration of mutans streptococci in the mother's or caregiver's saliva;
- The Transmission , i.e. the efficiency of the transfer: in this case the frequency of transmission from mother/caregiver to child;
- The Receiver , i.e. the ability of the target to receive the pathologic bacteria: in this case the presence of teeth in the child's mouth coupled with the availability of sugar in the child's diet to support the transfer.
Acid Production and Demineralization: Decay causing bacteria ingest sugar and other fermentable carbohydrates from the child's diet and produce acid as a by-product, causing a drop in the plaque pH. The acid attacks the outer surface of the tooth (enamel) after each food exposure (longer for sticky foods), resulting in mineral loss (demineralization). This is a highly sophisticated and dynamic process that is influenced by these bacterias' capacities to store carbohydrate substrate both intracellularly and extracellularly in the plaque for later metabolism into acid. For this reason, the decay process can continue unabated for an extended time between meals or snacks (although the greatest “decay attack” occurs during and for approximately 20 minutes after eating).
“White Spot lesions” - Clinically, these areas of demineralization are the first visually detectable signs of tooth decay. They are chalky white smooth patches or linear markings that most frequently form along the gum line where plaque is most abundant – starting on the maxillary incisors (upper front teeth). As they may be hidden under plaque, white spot lesions are most readily seen when the plaque is first wiped away using a corner of a washcloth or gauze square. (Finger cots made of terrycloth are available for cleaning babies' teeth.) Not all white spots are early lesions of tooth decay as some are developmental. Demineralized white spots resulting from tooth decay are unique in their flat appearance, shape, location, and association with plaque. Although white spot lesions represent loss of mineral from the tooth, the loss is localized mainly in the subsurface of the enamel. The enamel surface in this incipient lesion is essentially intact and amenable to remineralization. THIS STAGE IS REVERSIBLE IF CAUGHT IN TIME.
“Cavities” - When demineralization exceeds remineralization as a result of frequent or prolonged acid attacks, the result is a breakdown of the enamel and formation of a hole or “cavity” in the tooth surface. This is a late-stage sign of tooth decay. Cavities, unlike white spot lesions, are not reversible, but can be arrested with intense diet control and high frequency topical application of fluoride through a variety of products including toothpaste, rinses, and varnishes.
“Progression” - If the caries process is not suppressed or the cavity not repaired, the hole will continue to expand in depth and width. As it deepens, it moves inexorably toward the dental pulp (nerve) causing increased pain frequency and severity. When the pulp is directly affected by the caries process it dies and subsequently becomes infected. This infection first occurs within the nerve chamber of the tooth and then spreads beyond the tooth's root-end into the bone and soft tissues of the mouth and face. Unchecked, the infection can drain into the mouth (creating a parulis or fistula) or spread further into the neck, midface, and cranium. For this reason, draining abscesses and facial cellulites (infection of the cheek or other facial tissues) are common presenting signs of ECC. Numerous case reports of children presenting to the emergency room with facial cellulites “of unkown origin” turn out to be caused by dental infections.
Maria's reality |
Low income pre-schoolers are about twice as likely to experience caries, twice as likely to experience dental pain, have more than twice the extent of dental disease, and are about twice as likely to have insurance coverage because of Medicaid, but are only ½ as likely to have a dental visit because of lack of access (CDHP 38) |
To find out how Maria is treated and what the options are for managing her overall oral health, click on the link or picture below.
 |
 |
 |
 |
