
What is the role of fluoride? |
 |
Treatment
Learning Objectives
- Describe conventional treatment (restorative dentistry)
- Describe emerging treatment (Prevention and disease management)
|
Dual Approaches of Care at the Programmatic and Individual Levels |
|
In This Section
You will learn about the treatment of Maria. You will learn to distinguish conventional dental treatment (a restorative and “surgical” approach) from emerging disease management approaches (a behavioral and “medical” approach) along with their respective advantages and disadvantages.
Table of Contents
What is the classical treatment?
What is Disease Prevention?
Achieving Primary and Secondary Disease Prevention
What is Disease Management?
Delaying and Reducing Tooth Decay
Barriers to Care
What is the classical treatment?
|
Traditional Surgical Dental Repair Compared with New Medical Approaches |
“Drilling and Filling”
Conventional treatment involves surgically removing (by “drilling”) parts of the tooth that are damaged by tooth decay and restoring (by “filling”) those surfaces to their former form and function.
Typical filling materials used for repairing young children's teeth include “composites” (white fillings) amalgam (silver fillings), stainless steel crowns (caps), and pulpotomies (nerve treatments). This “surgical” treatment for ECC is often imposing on the young child, demanding on the dentist, and disconcerting for the parent. For this reason, many young children are treated in the operating room under general anesthesia. In the U.S., the initial cost of treating a child in the operating room for severe caries, exceeds 5 million dollars annually. (39)
By time children with ECC get to treatment, they often have such extensive decay that the upper incisors (front teeth) are beyond repair and need to be extracted, the molars need to be crowned (capped) to keep them intact, and additional teeth need fillings. The lower front teeth, however, are rarely affected because they are protected from exposure by the positions of the lip, tongue, and salivary glands.
The successful result of this extensive treatment typically looks like this:
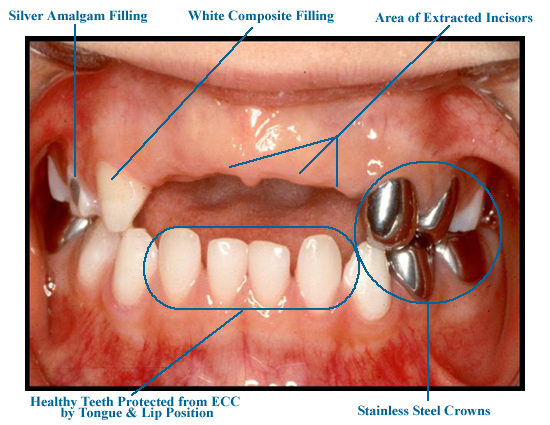
Does this mouth look like a success story?
While this repair immediately relieves Maria of her dental pain and infection and restores her ability to eat and sleep comfortably, it does little to address her underlying caries disease process. In fact, restorative dentistry alone has minimal impact on a child's ongoing caries susceptibility because it does not address the underlying caries process. For this reason, conventional dental repair should be considered more “prosthetic” than “therapeutic” and affected children often relapse - requiring ongoing dental repair to keep up with their ongoing active disease (40-43).
Early childhood tooth decay is a risk factor for future caries and is a good indicator of future caries experience (42, 44-46). Thus, the initial cost of treatment underestimates the long term cost associated with early child hood tooth decay. With the knowledge that tooth decay is an infectious and transmissible disease, that it is diet dependent and fluoride mediated, and that restorative dentistry has minimal impact on outcomes, the emerging trend in dentistry focuses on Disease Prevention and Disease Management.
What is Disease Prevention?
True Primary Disease Prevention: prevents disease occurrence by avoiding disease determinants. In tooth decay, this relates to reducing the reservoir of bacteria, reducing transmission and reducing colonization of cariogenic bacteria. (Reservoir -> vector -> receptor).can only occur before a child acquires sufficient cariogenic bacteria to develop tooth decay (i.e. before age 1) or later through stringent control of caries-promoting foods and eating behaviors.
Reducing the reservoir: Since the mother's (or primary caregiver's) saliva is the primary source of these bacteria, transmission can be reduced by limiting the concentration of cariogenic bacteria in the “donor's” mouth. Among agents that can reduce salivary levels are xylitol chewing gum, stannous fluoride, and chlorhexidine. Reducing maternal titers of cariogeneic bacteria is indicated only when the mother has had extensive decay experience.
Reducing transmission: Transmission occurs whenever saliva is directly transferred from the mother (or primary caregiver) to the child's mouth as happens when eating utensils are shared, a mother cleans a pacifier in her own mouth, or a mother uses her own saliva to clean around a child's mouth, The infant can also initiate the transfer by putting its hand in its mother's mouth and back into its own. The more frequent the transmission, the earlier these bacteria will make it from mother to child.avoid sharing utensils, cleaning pacifier in mouth etc.
Reducing colonization: Colonization of cariogenic bacteria is facilitated by presence of carbohydrates – especially simple sugar. Therefore, children who are allowed to use a bottle or sippy cup ad libitum containing almost anything except water are more easily colonized. Because fluorides inhibit cariogenic bacteria in many ways, fluoride varnish is particularly useful in reducing colonization in young children.
The University of Iowa's MCHB Leadership Training Program in Pediatric Dentistry provides information on fluoride varnish and its application. CDC maintains an interactive map showing states that have adopted fluoride varnish initiatives as part of their oral health programming. North Carolina was one of the first states to develop a comprehensive program around fluoride varnish. The North Carolina Academy of Family Practice provides extensive descriptive and training materials.
Tooth decay is a disease of im balance between Pathogenic Factors and Protective Factors. When the mouth is in a state of health, the pathogenic factors are balanced by protective factors so that no cavities result.
Achieving Primary and Secondary Disease Prevention
Primary disease prevention may be achieved with early intervention and anticipatory guidance:
Anticipatory guidance - Anticipatory guidance is an approach to child care that guides parents to take actions that promote their children's health in anticipation of conditions that could be deleterious.
Early childhood oral health anticipatory guidance resources:
- MCHB Oral Health Resource Center: Pediatric Oral Health Guide
- MCHB Oral Health Resource Center: Open Wide
- American Academy of Family Physicians: Anticipatory Guidance in Infant Oral Health
- American Academy of Pediatrics: Oral Health Risk Assessment Training
- Bright Futures: Oral Health
- The Association of Clinicians for the Underserved: Clinician's “Pocket Cards”
- American Academy of Pediatric Dentistry: Guidance on Periodicity, Prevention, Anticipatory guidance, and Treatment
Dental Home - The concept of the “dental home” by the American Academy of Pediatric Dentistry is derived from the American Academy of Pediatrics concept of the “medical home” . It brings together parents, children, and caregivers to offer timely and effective anticipatory guidance, preventive interventions and comprehensive care, including referrals to other providers as needed.
Age One Dental Visit - Because tooth decay is established as a disease process during a child's first years of life, early preventive intervention is essential – particularly for children at high risk of ECC . Both AAPD and AAP have official policies in support of early dental visits.
The pediatrician's policy statement emphasizes the need for primary medical care providers to refer children identified at high risk for dental caries while the pediatric dentists' statement calls for universal dental care at age one. An analysis of the pros and cons of these policy differences in terms of public health suggests that the more targeted approach holds stronger potential for allocating resources most efficiently. The cost effectiveness of early interventions has been modeled by investigators using two different approaches, cost-estimation model and cost-effectiveness model, and demonstrated using North Carolina's Medicaid claims. According to a CDC analysis, costs of prevention-oriented care are far lower than costs of traditional dental repair in the hospital operating room.
Secondary Disease Prevention: prevents disease by maintaining a state of balance between disease and health after the risk factors for disease are already present. For dental caries, this is accomplished by maintaining balance between pathologic factors that lead to demineralization of the tooth and protective factors that lead to remineralization of the tooth. A state of oral health is not absence of activity, but rather a balance of activity as the teeth are either de- or re-mineralizing at every moment. When demineralization exceeds remineralization, the tooth will first demonstrate a “white spot lesion” (the earliest clinical signs of tooth decay). If demineralization continues to exceed remineralization this reversible lesion will continue to a full-fledged cavity and on to a toothache, dental abscess, and abscess of the surrounding bone and face.
What is Disease Management?
When children have not had the benefit of primary prevention and anticipatory guidance, and caries activity has progressed to the point that there is tooth destruction, the following concepts are employed:
Disease Suppression: this is the complete suppression of caries activity leading to a state of “arrested caries”. Once complete suppression is obtained the disease process is inactive and the teeth “do their best” to remineralize. As a result, the white spot lesions fade away, the decayed tooth material in the cavities turns from a light brown to dark, the edges of the cavities will stop spreading and become very distinct, and the gum tissue becomes firm and pink. Where the decayed tooth structure has been removed by “excavation” (scraping), the healthy dentin (the deeper layer of tooth material below the white enamel) will show through as yellow and glassy. The child will become asymptomatic to stimuli that were previously painful - like air flow (breathing across the affected tooth), and hot and cold foods.
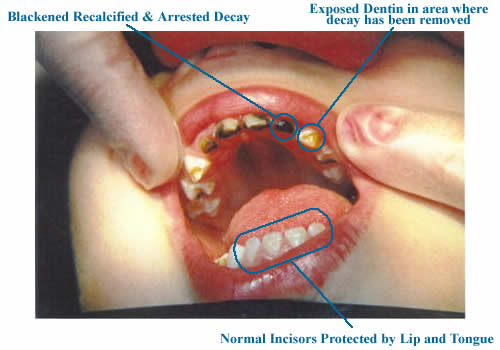
Arrested ECC in a 2 Year Old
Disease Arrest: Gaining caries arrest involves intensive diet control to reduce frequency of acid attack on teeth, high-fequency, low-dose fluoride applications to increase remineralization and resistance to attack and gross caries excavation to decrease bacterial load and allow the fluoride to reach the leading edge of the progressing decay. Once caries activity has been completely suppressed, affected teeth will have lost tooth structure (“cavity”) but will not need to be restored except to restore function and esthetics. If parents are able to sustain a state of caries arrest in their young children, surgical/restorative dentistry can be delayed until a child is old enough to well tolerate dental treatment without use of general anesthesia. ill not need to be restored unless it is an issue of function or esthetics.
The following two diagrams portray the demineralization and remineralization processes as phenomena fed by the “heat” of a cariogenic diet and reversed by the “cooling” of fluoride and salivary minerals.
Delaying and Reducing Tooth Decay
Delaying and reducing transmission of cariogenic bacteria can prevent cavities in young children. Among children who do get cavities, these strategies delay timing of the first cavity and reduce the total amount of tooth decay the child will develop. Mother-child couples receiving prenatal counseling on oral health and preventive care (dental cleanings and fluoride applications) every 6 months, had a significant improvement in oral health and a reduction of mutans streptococci during the 4 year study period. Children enrolled in the study from before birth to 4 years of age, that received preventive treatment had a reduced caries incidence and delayed S. Mutans colonization (51). In a series of classic Scandinavian reports of a longitudinal case-control study by Bridgette Kohler, reducing mutans reservoirs in mothers delayed children's acquisition of cariogenic bacteria and lowered their decay experience.
Prevention of oral disease, whether it is periodontal disease or tooth decay, will not work if the populations at risk can not access care.
Barriers to Care
What are the common barriers to care?
- Low socioeconomic status
- Lack of community programs (e.g water fluoridation)
- Logistic barriers (transportation, conflict with work, child care, physical disability)
- Lack of resources to pay for care/lack of dental insurance
- Inadequate public dental insurance programs and low provider participation
- Lack of public awareness and understanding of the importance of oral health
Specific action steps can be taken to increase oral health awareness and access for high risk populations.
 |
 |
 |
 |