HIV in Swaziland
In 2003, Swaziland was a small, poor southern African nation with a population of just over a million in an area not much larger than the US state of Connecticut. Swaziland was listed as a lower-middle income country, but it had a high level of inequality. Two thirds of the population lived below the poverty line, subsisting on less than a dollar a day, and women accounted for two thirds of the poor. [18] For pregnant women, HIV prevalence was 39 percent. [19] Life expectancy had plummeted to 43 years, with HIV-AIDS the leading cause of death by far.
Swaziland also had entrenched cultural practices that contributed to the spread of HIV-AIDS. For example, Swazis valued large families, and women were expected to have at least five children. Men largely controlled women's reproductive decisions. One long-established custom was for a man to marry his brother’s widow. In fact, one study found that Swazis considered monogamy, family planning and birth control to be foreign practices. [20] King Mswati III, the country’s monarch and ruler, was a case in point. He had more than a dozen wives. The king’s father, Sobhuza II, had 70 wives and more than 200 children when he died in 1982 after a 60-year reign. [21] Polygamy and promiscuity were not uncommon in sub-Saharan Africa generally, but the scale of the behavior in Swaziland posed a particular challenge.
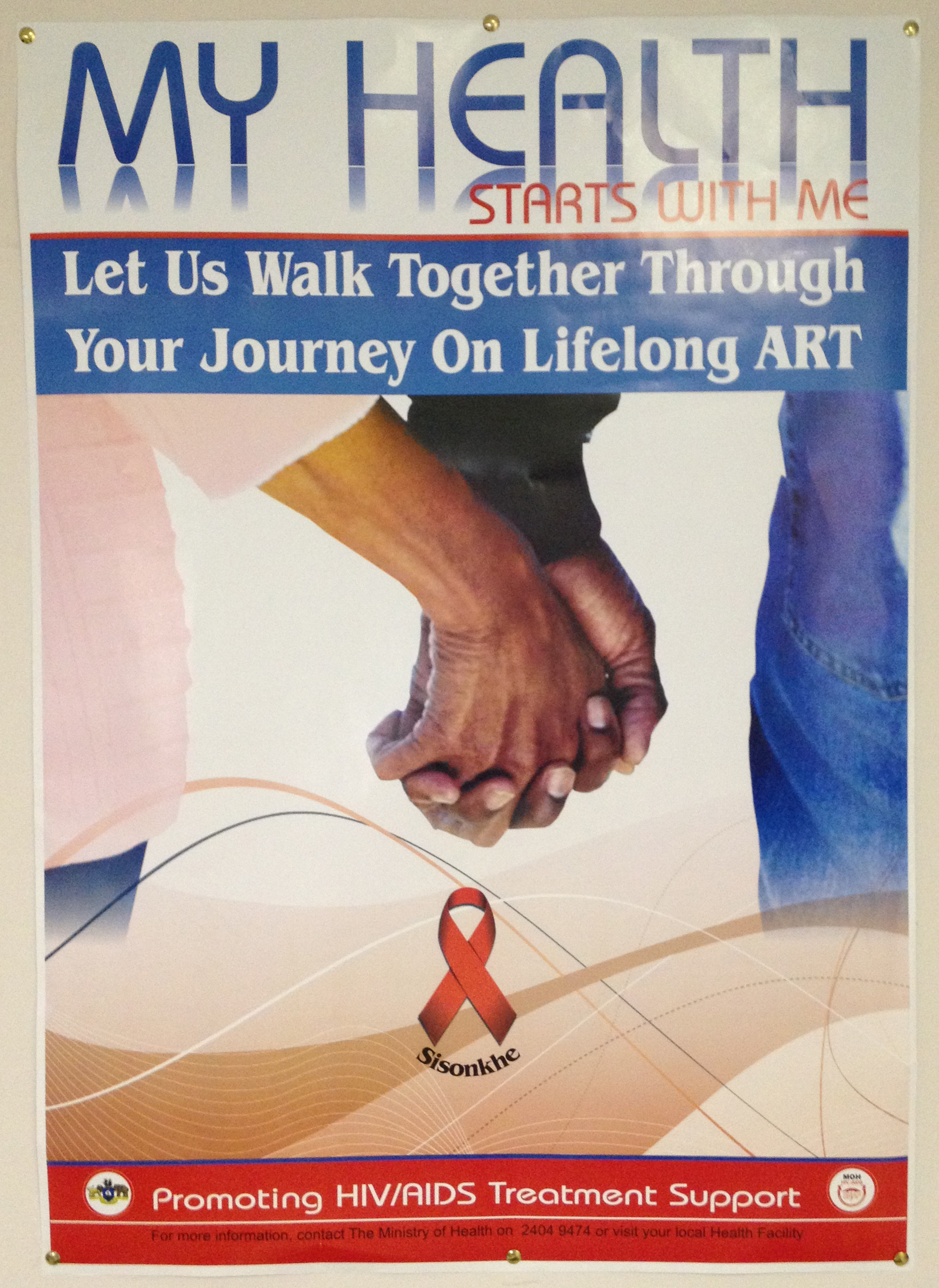
SNAP PSA Poster
As far back as 1987, the government had created the Swaziland National AIDS Programme (SNAP) to coordinate the health sector response to the epidemic. In 2001, it added the National Emergency Response Council on HIV/AIDS (NERCHA) to coordinate the national response across sectors, set the country’s HIV-AIDS strategy, and channel money from the government and international community to implementing organizations such as SNAP. [22] Beginning in June 2003, Global Fund began providing funds to Swaziland for the purchase of antiretroviral drugs, and in November the Elizabeth Glaser Pediatric AIDS Foundation created a partnership with the Ministry of Health to provide PMTCT services. [23] The same year, SNAP created the National ART Programme to deliver antiretroviral treatments and overall care. [24]
Then, in February 2004, the government formed a Technical Working Group (TWG) to monitor programs, debate research protocols and treatment regimens, and advise the government on HIV-AIDS policy. The group consisted of some 30 specialists, chaired by Ministry of Health staff and including representatives of international organizations working on HIV-AIDS in Swaziland. The government realized the country had reached a critical mass of international and domestic expertise, and was in a position to chart its own way forward through the crisis.
[18] About UNDP in Swaziland. See http://www.sz.undp.org/content/swaziland/en/home/operations/about_undp.html
[19] WHO website. See: http://www.who.int/hac/crises/swz/Swaziland_Aug05.pdf
[20] “Swaziland: A culture that encourages HIV/AIDS,” IRIN , April 15, 2009. See: http://www.irinnews.org/report/83937/swaziland-a-culture-that-encourages-hiv-aids
[21] Dana Hughes, “Life of a Swazi King: Bare-Chested Brides and Rolls Royces,” ABC News , January 28, 2009. See http://abcnews.go.com/International/AroundTheWorld/story?id=6480460
[22] National Emergency Response Council on HIV and AIDS (NERCHA) website. See: http://www.nercha.org.sz/
[23] Elizabeth Glaser Pediatric AIDS Foundation Call to Action Project, Semi-Annual PMTCT Program Report October 2003-March 2004 . See: http://aidstar-one.com/sites/default/files/promising_practices/g3p_docs/CTA-Semi-Annual-Program-Report-Oct-03-Mar-04.pdf
[24] Swaziland National HIV/AIDS Programme. See: http://www.gov.sz/images/stories/Health/swaziland%20national%20aids%20programme.doc